I recently attended Stephen Porgues workshop in Ottawa called Social Connectedness as a Biological Imperative: Understanding Trauma through the eyes of Polyvagal Theory. If anyone is interested in pursuing a specialization in trauma or expanding their trauma learning repertoire, I highly recommend attending a workshop with Stephen Porgues. He is a great speaker that can break down the science of Polyvagal Theory so that you can apply this knowledge to helping your trauma clients. It was a very informative and even inspiring workshop to attend. I cannot say all workshops in the past have given me more fuel for the passionate work that I feel I am doing. I thought I would share some insights and learning points that I took away from this workshop. By all means, it would be wise to look into Polyvagal Theory in its entirety to full understand its scope and application for treatment. I will not be going into it in full as that would take up a lot of blog space and it is not the purpose I intend on in my blog. I recommend either attending a workshop or purchasing Stephen Porgues book on Polyvagal Theory.
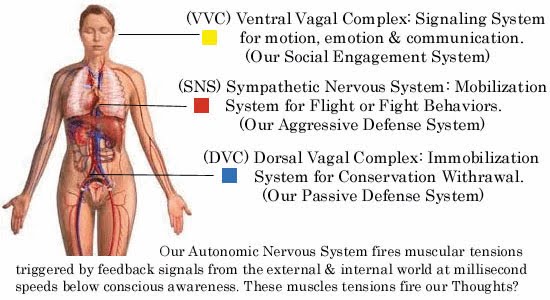
First of all, Polyvagal Theory specifies two functionally distinct brances of the vagus nerve, the tenth cranial nerve, that serve different evolutionary stress in mammals, including us humans. The less evolved vagus nerve branch serves as a more primitive branch that illicits immobilization behaviors (ie feigning death) whereas the more evolved vagus branch is linked to social communication and self soothing behaviors (wikipedia). You can check out YouTube for more explanations on Polyvagal Theory – here’s another brief definition in relation to trauma https://www.youtube.com/watch?v=8RKC3Ga6shs Polyvagal Theory claims that the nervous system employs a hierarchy of strategies to both regulate itself and to keep us safe in the face of danger. In fact, it’s all about staying safe. Our highest Strategy involves social engagement which is regulated by the myelinated vagus nerve. Our next strategy is fight or flight, regulated by the sympathetic nervous system when social engagement is not an option. Our last option is to freeze, to immobilize when fight/flight is not an option in the face of trauma(Garland, 2013).
Here are some learning points I’d like to share:
- Our culture is behaviourly oriented. That means there is a lot of shame associated with immobilization or freezing during a traumatic event. Society says you “should” fight or run (fight/flight); however, in trauma that is not always an option. To stay safe in an extreme circumstance, some individuals have to immobilize. This is where rape victims might freeze in order to survive. There should not be any shame associated with this because Stephen Porgues states that we do not have control over how we handle a trauma as it unfolds. Our bodies know what to do before our mind understands. It’s our primitive reaction. Their is a lack of control over how you will respond. This can help vindicate some clients from their shame.
- In order to co-regulate with another person, we need certain social engagement behaviors to feel safe with that person. Engagement turns off defenses.There are 3 behaviors: Facial expressions, gestures and prosodic vocalizations (intonation of voice the higher more soothing the voice the more safer perceived). Eye gaze can be seen as a threat at times for some trauma clients but prosody of voice is more of a stronger behavior for eliciting safety. Therapists can be mindful of all three behaviors in their therapy sessions with clients.
- Humans need others because regulators of physiology are embedded in relationships.
- Deep breathing can help regulate as well. Take a deep abdominal breath and exhale slowly. Teaching clients this can be valuable; however, not every trauma client will be prepared to learn this technique early on. If clients are willing, pranayama yoga, which is breathwork in yoga, may be of benefit to helping regulate their physiology and enables repair of the social engagement system. Music shares features with the human voice and can help regulate as well.
- Trauma clients have difficulties in co-regulation: feeling safe with others, being in physical proximity with others, being touched or touching others and establishing trust in their social relationships. These are hallmarks for treatment outcomes. The main neural circuits that optimize behavioural defense, disrupt the circuits that maintain physiological and mental health.
Again, I encourage those who are interested to review more of the neurobiology of the vagus nerve in the Polyvagal Theory to understand typical behaviors that some trauma clients may exihibit. We become better therapist when we can fully understand the biology of behavior.
Andrea Cashman is a registered psychotherapist in private practice who has founded Holistic Counselling Services for individual clients seeking therapy in Ottawa, Ontario. She also practices at The Ottawa Hospital as a registered nurse. Feel free to comment below or contact her at [email protected] or visit her website at www.holisticcounsellingservices.ca
References:
https://en.wikipedia.org/wiki/Polyvagal_Theory
https://www.youtube.com/watch?v=8RKC3Ga6shs
Garland, T. (2013) Polyvagal Theory, Sensory Challenge and Gut Emotions
*The views expressed by our authors are personal opinions and do not necessarily reflect the views of the CCPA